How Naloxone Co-Prescribing Laws Can Facilitate Opioid Education
Legislation regarding naloxone and opioid co-prescribing laws may facilitate opioid education by allowing healthcare professionals to discuss the risk of opioid use and emergency overdose care.
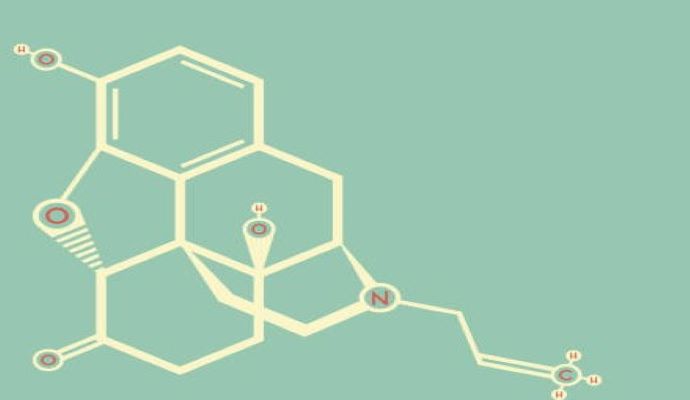
Source: Getty Images
- Fueled by deceit from pharmaceutical companies and over-prescription, the opioid epidemic has continued to impact thousands of lives. Throughout recent years, public health organizations and healthcare professionals have been working to implement practices to reduce opioid use disorder (OUD) and prevent overdoses. One of the newest risk mitigation strategies has been enforcing naloxone co-prescribing laws, which can facilitate opioid education, widen treatment access, and minimize the unfavorable outcomes associated with an opioid prescription.
A Brief Background
Since the push for opioid prescription by pharmaceutical companies in the late 1900s and false claims about their safety, the opioid epidemic has been a primary concern in the United States. What clinicians now understand about opioids is that they are highly addictive substances that should be prescribed with caution after assessing the prescription's benefits and concurrent risks.
Despite the understood risks of opioids, they continue to be effective pain management tools for many clinicians. Data from the CDC notes that despite the lowest rate of opioid prescriptions in 15 years, the 2020 opioid prescription rate was as high as 43.3 prescriptions per 100 individuals, amounting to over 140 million prescriptions overall.
The subsequent outcomes of these prescription rates are high incidences of OUD and opioid-related overdose. In fact, the CDC notes that nearly 75% of drug overdoses in 2022 involved an opioid. Between 1999 and 2020, over 263,000 people in the United States died from opioid-related overdoses. The National Institute on Drug Abuse (NIDA) also notes that 21–29% of people with an opioid prescription will abuse them.
Naloxone
Understanding the severity of the opioid epidemic, many public health organizations have advocated for expanded access to naloxone — sometimes known as Narcan — a rescue medication that can sometimes reverse the effects of opioids.
According to the NIH, naloxone is an opioid antagonist that binds to opioid receptors, preventing other opioids from binding and affecting the patient. In many cases, naloxone can restore breathing that has ceased or slowed during an opioid overdose. Delivered as a nasal spray or injection, naloxone has no impact on patients who do not have opioids in their system.
Naloxone Prescribing Legislation
Caroline Collins, a Senior Behavioral Health Implementation Specialist at Sunwave, told PharmaNewsIntelligence that there are limited federal regulatory laws surrounding naloxone prescription. While different federal health organizations recommend Narcan to help minimize the risk of overdose, legislation falls to individual states.
General Guidelines
Collins told PharmaNewsIntelligence that the FDA and CDC guidelines recommend that physicians co-prescribe naloxone — also referred to as Narcan — whenever they are prescribing an opioid or opioid use disorder medication, such as methadone or suboxone.
“They should also be receiving education on how to use Narcan,” added Collins. She notes that the CDC specifically comments that every household with someone who takes an opioid or an opioid use disorder medication should have Narcan on hand.
Despite many public and private healthcare organizations recommending co-prescribing, there are few regulatory guidelines.
State Legislation
“All 50 states have now enacted access laws, which means that patients don't need a prescription to obtain naloxone,” noted Collins. “They can go into pharmacies and pick it up. However, there are varying costs depending on the state and how a patient obtains it.”
In addition to the current access laws, many states have or are considering implementing co-prescribing regulations. Collins noted that New York is joining ten other states, including Virginia, Vermont, Arizona, Florida, Ohio, Rhode Island, Washington, California, New Mexico, and New Jersey, in enacting a co-prescribing law.
“Those are varied in terms of their specificity on why providers would prescribe it,” she commented. “New York co-prescribing laws are rather broad.”
According to Collins, in New York, anyone who receives an opioid pain medication for maintenance of pain issues should receive a naloxone prescription the first time they receive their prescription. If needed, the patient can also get refills throughout the year.
Collins notes that this legislation’s primary goal is to reduce the number of overdoses in each state.
“In states where people obtain Narcan, whether walking up to a physician or a pharmacy and asking for it or receiving it as a prescription, we see overdose trends down. So it appears to be working, regardless of how we're getting it into people's hands,” emphasized Collins.
Co-Prescribing and Education
Collins explained that one of the most significant benefits of co-prescribing is the opportunity to educate patients on opioids, OUD, and overdose safety. “We're asking physicians to be more forthcoming about the potential of abuse, addiction, and overdose with opioids,” she notes.
Beyond educating patients on opioids and addiction, co-prescribing allows providers to teach patients how naloxone can be used and emphasize that emergency services should be called when naloxone is administered.
“If somebody is then going to the hospital or receiving follow-up medical services, that's an intervention opportunity,” noted Collins. “However, we don't want somebody to suffer an overdose to receive services. But the fact that we're educating the community to utilize Narcan in this way, and we can assume that they will interact with healthcare systems immediately following that, is important.”
Continuing Educational Efforts
“We can look at other campaigns that have been related to public health, such as Stop the Bleed, some of the smoking cessation campaigns that we see on our TVs, and things like that,” replied Collins when asked how we can enhance general educational efforts on naloxone.
She lists multiple methods, including traditional media campaigns, social media, and provider education efforts. Public health professionals may consider educating through various means depending on the target demographic. Collins noted that education goes a long way in ensuring that patients and families understand how to use Narcan and where to get it.
In addition to legislation enforcing co-prescribing, Collins urges individuals in healthcare systems to revise internal policy and encourage the co-prescribing of Narcan. “In most healthcare organizations I've interacted with recently, she explained that Narcan is a part of the training curriculum, either yearly or biannually,” she explained.
“The FDA and CDC make very clear their recommendations that co-prescribing is the next step from the access laws. If that were at a federal level, it would create consistency so that we don't have to rely on states to manage their trends, and we can address this at a federal level,” concluded Collins.
